It’s winter and the winter vomiting bug is back in action. The bug’s scientific name is Norovirus and is the main cause of acute gastroenteritis worldwide. You surely would have experienced the effects of this bug, especially if you have children going to school! If you want to know more about this bug, this article is just for you!
Introduction
Non-bacterial diarrheal illnesses have been studied, for a long time, to understand their cause and pathogenicity. Beginning in the late 1960s to the early 1970s, the absence of bacteria in acute gastroenteritis cases had intensified the search for viral etiologic agents. The rationale for viruses being a causative agent included the unknown etiology of the infectious outbreaks, absence of bacteria, and the ability of bacteria-free stool filtrates to transmit infection in adult volunteer studies [1].
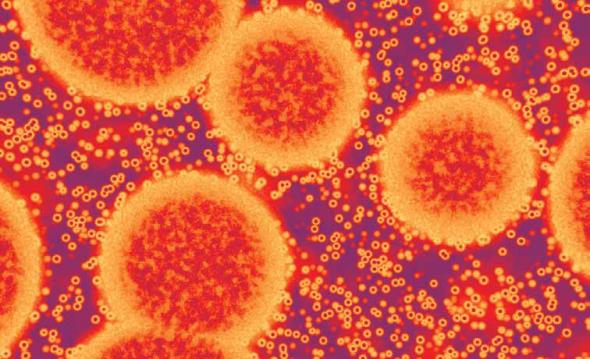
In October 1968, an outbreak occurred in an elementary school in Norwalk, Ohio, where 50% students and teachers developed gastroenteritis. The illness typically lasted 24 hrs, and was similar to that described by Zahorsky in 1929 [2]. However, studies by the Centres for Disease Control in 1970, failed to isolate an etiological agent. In 1972, Kapikian undertook electron microscopy to study fastidious, non-cultivable organisms, especially viruses. Stool samples containing the Norwalk agent were examined, using convalescent serum from a volunteer as the antibody. Glistening aggregates of non-enveloped, antibody-coated, 27 nm virus-like particles were visualized (Fig 1). Further studies determined that the virus-like particle was indeed the etiological agent of the Norwalk outbreak [3], and was thus renamed the Norwalk virus, the only known species of the genus Norovirus at that point in time.
Fig 1. Visualisation of Norovirus particles by electron microscopy (left panel) and X-ray chrystallography of a single virus particle (right panel).
Norovirus belongs to the Calciviridae family of viruses. It is also known as the “winter vomiting bug”. Although outbreaks are known to occur year round, they tend to peak during the cold season [4]. Norovirus is globally recognized to cause acute viral gastroenteritis, and is responsible for a number of outbreaks [5]. It is highly infectious, and is responsible for person-to-person transmission [6]. Its ability to survive in aerosols enhances the risk of environmental contamination, and further facilitates spread of the disease. Closed environments further aid outbreaks, which have frequently been reported in healthcare centres, childcare facilities, hospitals, ships and prisons. Although direct transmission is the major mode of dissemination, viral infections also occur through ingestion of contaminated food and water, and also by touching contaminated surfaces [7, 8]. Human Noroviruses are responsible for < 95% of nonbacterial gastroenteritis outbreaks [9, 10].
Structure of Norovirus
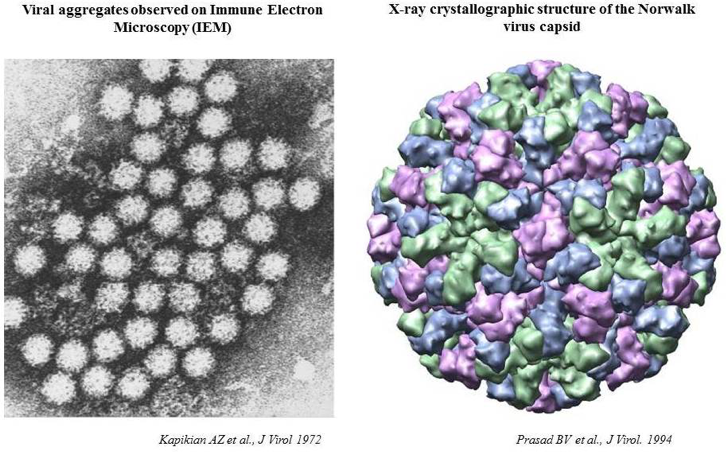
The virus has a non-enveloped structure, consisting of a capsid and nucleic acid, measures 38-40 nm in diameter, and has a T=3 icosahedral symmetry. The capsid is composed of 180 VP1 proteins. The small, empty capsids measure about 23 nm, with a T=1 icosahedral symmetry, and 60 VP1 proteins (Fig 2). The 3D structure is exhaustively described by Prasad and colleagues [11].
Fig 2. Diagrammatic representation of Norovirus structure
Image Source: http://viralzone.expasy.org/all_by_species/194.html
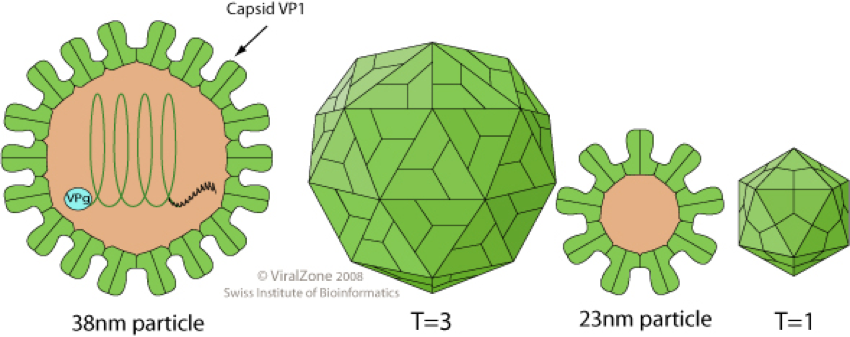
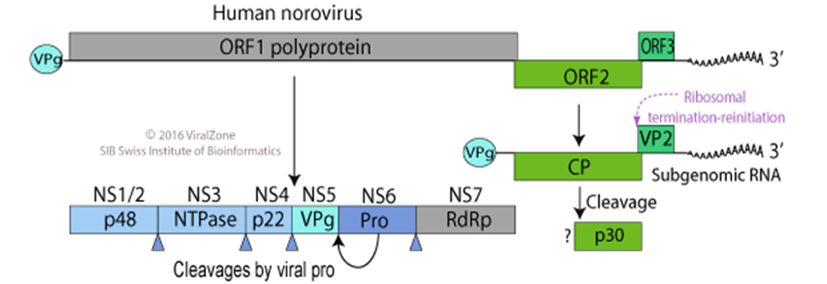
Noroviruses have a linear, single stranded RNA genome of 7.3 to 8.3 kb, exhibiting a positive polarity (ssRNA(+) genome). The genome is covalently attached to a virus-encoded protein (VPg) at the 5’ end, whereas the 3’ end is polyadenylated. The UTRs at either end are short, and contain evolutionarily conserved structures, which are important for viral replication, translation and pathogenesis. The genome has three open reading frames (ORF). ORF1: translated into a non-structural, 194-kDa polyprotein, cleaved by virus protease 3C into probably 6 proteins, including the RNA-dependent RNA polymerase. ORF2 and ORF3: translated from subgenomic RNA, encoding the major (VP1) and minor (VP2) capsid proteins, respectively. Being identical to the last 2.4 kb of the genome, the subgenonic RNA is similarly attached to VPg at the 5’ end, and having a polyadenylated tail at the 3’ end (Fig. 3) [12].
Fig 5. Schematic representation of Norovirus genome structure
Image Source: http://viralzone.expasy.org/all_by_species/194.html
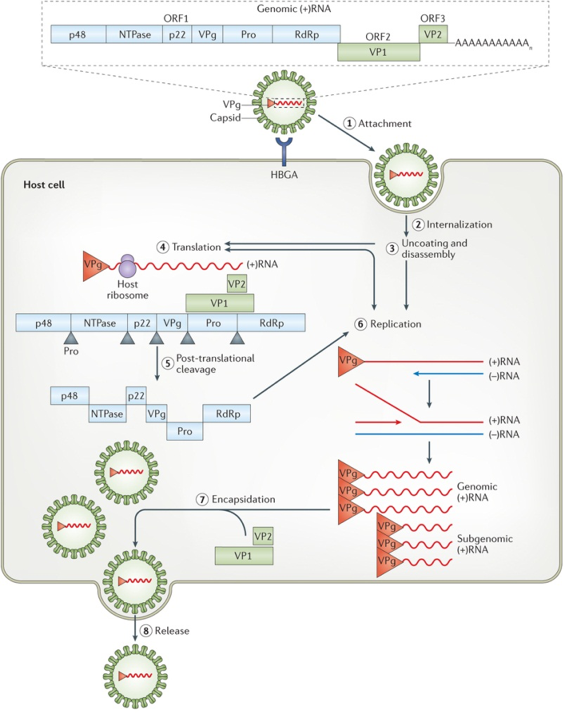
The life cycle and replication of the Norovirus
Noroviruses have a prolonged infection period. The short lag or incubation period could last up to 2 days, between the time of infection and onset of symptoms. People remain contagious during the incubation period, during the course of the disease, and 48 – 72 hrs after symptoms resolve. Some patients, who have a compromised immune system, can shed the virus for few months.
The viral capsid (VP1) attaches to the host histo-blood group antigens (HBGAs) present on the cell surface (step1). Subsequently, the virus is internalized, uncoated and disassembled (steps 2, 3). Host translation factors recruited by the non-structural VPg protein enables the transcription and translation of the viral (+)RNA in the cytoplasm of the host cell (step 4). Following translation, the polyprotein encoded by ORF1 is cleaved by the virus encoded protease (Pro, also known as NS6 or 3C-like) into 6 individual (non-structural) proteins (step 5). During replication, the (+)RNA is transcribed into negative-sense RNAs ((−)RNAs). These form the templates for the synthesis of new genomic and subgenomic (+)RNAs, respectively (step 6). The subgenomic (+)RNAs contain only ORF2 and ORF3, and are used for the production of VP1 and VP2. The newly synthesized viral RNAs are assembled into new virions, in the process known as encapsidation (step 7). The newly synthesized virions are then released from the infected host cells (step 8), by an unknown mechanism [13].
Fig 4. Life Cycle of Norovirus
Image source: http://www.nature.com/nrmicro/journal/v14/n7/fig_tab/nrmicro.2016.48_F1.html
Clinical Disease and Genetic Diversity
There has been a spate of norovirus outbreaks in recent years. Although this virus is very difficult to study and a lot remains to be understood, numerous advances have greatly contributed in comprehending this disease. In this section, we will briefly discuss the clinical disease and genetic diversity of norovirus [14].
Clinical Disease
Norovirus has a typical incubation period of 24–48 hrs, with disease resolution within 12–72 hrs. Acute gastroenteritis is the typical outcome of the disease, with symptoms including vomiting and diarrhoea, which may be accompanied with nausea and severe abdominal cramps. Although the disease normally resolves in a few days, it can be severe and prolonged in certain risk groups, such as infants, young children, transplant patients, and other severely immunocompromised patients. Bloody diarrhoea has been reported in norovirus infections in inflammatory bowel disease patients.
The global morbidity associated with this disease has been difficult to assess due to certain inherent properties of the virus. Noroviruses are difficult to propagate and are genetically variable. Hence, their detection by cell culture and RT-PCR-based detection assays is complicated. Secondly, there is a lack in the disease being reported to health officials, due to its acute nature. Most importantly, there is no standardization of any diagnostic or surveillance schedules. However, recent recognition and awareness of the disease has resulted in significant improvements in diagnostic assays and the needs for standardization protocols.
With improved diagnostics, norovirus infections have been reported in association with clinical outcomes, other than gastroenteritis. These include encephalopathy, intravascular coagulation, necrotizing enterocolitis in premature infants, postinfectious irritable bowel syndrome, and benign infantile seizures.
Genetic Diversity
Noroviruses are classified in five genogroups (GI-GV). The human viruses are primarily contained in genogroups GI, GII, and GIV. The genogroups are further sub-divided into 31 genotypes (8 GI, 19 GII, 2 GIII, 1 GIV, and 1 GV genotypes). Strains are typically named after the place/location where they were first identified. Excessive genetic variability is seen among noroviruses: members within a genogroup differ by 45–61% in their capsid genes, members within a genotype differ by 14–44%, and strains within a genotype differ by 0–14%.
Pathogenesis and Immunity
As discussed earlier, infections are predominantly caused via the oral route. The virions withstand acidic pH, and therefore survive passage through the stomach. Previous studies reported the infectious nature of noroviruses to be a combination of low infecting doses (DI 50 < 20 virus particles), high virus excretion level (108 to 1010 copies of RNA per gram of feces), and extended excretion after clinical recovery. There have been reports of asymptomatic infections, and shedding of the virus can continue up to 2 weeks after symptoms have disappeared. Although chronic infections are unknown, immunosuppressed patients have been known to shed the virus for over 8 months [15].
Due to the inability to culture the viruses and lack of an animal model, in vitro neutralization assays could not be developed; hence, data on immunity development is obtained from human volunteers. Studies indicate development of short-term homologous immunity, which correlates with the serum antibody levels. Although a candidate vaccine has been developed, it is as yet unknown whether it induces homotypic or heterotypic immunity. Due to the lack of suitable preventive or control methods, the development of a vaccine is the need of the hour [15].
Prevention
About 20 million people suffer from Norovirus infection each year. Being a highly contagious virus, most infections occur due to close contact with patients or due to ingestion of contaminated foods. About 70% outbreaks caused by contaminated foods are due to improper handling of foods by infected workers. Outbreaks are frequently associated with closed environments, which facilitate the person-to-person spread. Norovirus infection is generally manifested with vomiting and severe diarrhoea. The virus can survive in aerosols, and dried vomitus, if left uncleaned, helps in dissemination of the pathogen. Similarly, unhygienic handling of food by infected workers enables a spread of the disease [6, 7, 8].
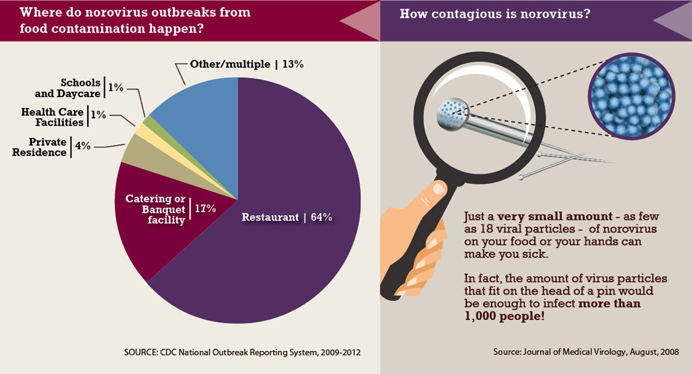
The infographic below helps us to understand the most prevalent places for outbreaks, and the contagious nature of the virus (Fig. 5). Since just a few virions are capable of causing the disease – as few as 18 viral particles – it is imperative that a high degree of hygiene should be maintained to prevent any unwanted outbreaks.
As seen in Fig 5, restaurants are the major hubs of norovirus outbreaks (64%). Thus, the food industry needs to maintain strict guidelines to prevent gastrointestinal outbreaks. Billions of virions are shed in stools and vomit of infected individuals. However, it should not be forgotten that virus dissemination also occurs before and after the infection, when the individual is asymptomatic. Thus, workers should ensure and practice proper hand washing, desist from handling raw fruits and vegetables with their bare hands, staff should be certified and trained in food safety practices, and most importantly, all sick workers should be required to stay home [16].
Fig 5. Infographic of Norovirus outbreaks
Image Source: http://CDC National Outbreak Reporting System, 2009-2012
A general practice to prevent any unforeseen infections would include the following (Fig 6) [17]:
- Proper hand hygiene: wash hands thoroughly with soap and water, especially after using the toilet, changing diapers, and always before eating, handling or preparing food
- Proper washing of fruits and vegetables. Contaminated foods should be discarded
- Cook all seafood thoroughly. Norovirus are relatively heat resistant, and are known to survive temperatures of 140°F (60°C). Hence, cooking shellfish by steaming may be insufficient to kill the virus
- Do not prepare food or provide healthcare for at least 48 hrs after recovery. Kitchen staff in the food industry should be given different duties to prevent any unwanted contaminations
- All contaminated surfaces (eg. after diarrhea or vomiting) should be immediately and thoroughly cleaned. Bleach or disinfectants should be adequately applied
- Soiled and contaminated clothes and linen should not be handled with bare hands. Wash well with detergents and maximum wash cycle, followed by machine drying. Wash hands thoroughly after handling soiled items
The CDC has issued a detailed guideline [18] for healthcare centres, which can be accessed at https://www.cdc.gov/hicpac/pdf/norovirus/Norovirus-Guideline-2011.pdf
Fig 6. Preventive measures against Norovirus infection
Image source: Journal of Medical Virology, August, 2008
Conclusion
Norovirus infection is a self-limiting illness, typically lasting for 2-3 days. The ease of transmission and low viral load required for infection is the cause for extensive outbreaks. The fastidious nature of the organism has hindered the quest for suitable diagnostics and preventive vaccine. The best way to prevent outbreaks is by maintaining and following good, personal hygiene.
References
- Kapikian, A.Z. The Discovery of the 27-nm Norwalk Virus: A Historic Perspective. The Journal of Infectious Diseases 181 (Suppl 2):S295–302 (2000).
- Zahorsky, J. Hyperemesis hiemis or the winter vomiting disease. Arch Pediatr 46:391–5 (1929).
- Kapikian, A.Z., Wyatt, R.G., Dolin, R., Thornhill, T.S., Kalica A.R., Chanock, R.M. Visualization by immune electron microscopy of a 27 nm particle associated with acute infectious nonbacterial gastroenteritis. J Virol 10:1075–81 (1972).
- Lopman, B.A., Reacher, M., Gallimore, C., Adak, G.K., Gray, J.J. and Brown, D.W.G. A summertime peak of “winter vomiting disease”: Surveillance of noroviruses in England and Wales, 1995 to 2002. BMC Public Health 3:13 (2003).
- Lopman, B., Zambon, M. and Brown, D.W. The evolution of norovirus, the “gastric flu”. PLoS Med 5:e42 (2008).
- Teunis, P.F., Moe, C.L., Liu, P., et al. Norwalk virus: How infectious is it? J Med Virol 80:1468-76 (2008).
- Goodgame, R. Norovirus gastroenteritis. Curr Gastroenterol Rep. 8(5): 401–08. (2006).
- Said, M.A., Perl, T.M., Sears, C.L. Healthcare epidemiology: gastrointestinal flu: norovirus in health care and long-term care facilities. Clinical Infectious Diseases 47 (9): 1202–8 (November 2008).
- Billgren, M., Chistenson, B., Hedlund, K.O., and Vinje, J. Epidemiology of Norwalk-like Human Caliciviruses in Hospital Outbreaks of Acute Gastroenteritis in the Stockholm Area in 1996. Journal of Infection Volume 44, 26-32 (2002).
- Fankhauser, R.L., Noel, J.S., Monroe, S.S., Ando, T., and Glass, R.I. Molecular Epidemiology of “Norwalk-like Viruses” in Outbreaks of Gastroenteritis in the United States. Journal of Infectious Diseases Volume 178, 1571-1578 (1998).
- Prasad, B.V., Rothnagel, R., Jiang, X., Estes, M.K. Three-dimensional structure of baculovirus-expressed Norwalk virus capsids. J Virol 68(8):5117-25 (Aug 1994).
- Thorne, L.G., and Goodfellow I.G. Norovirus gene expression and replication. Journal of General Virology 95, 278–291(2014).
- de Graaf, M., van Beek, J. Koopmans M.P.G. Human norovirus transmission and evolution in a changing world. Nature Reviews Microbiology 14, 421–433 (2016)
- Karst, S.M. Pathogenesis of Noroviruses, Emerging RNA Viruses. Viruses 2, 748-781; doi:10. 3390/v2030748 (2010).
- Morillo, S.G. and Timenetsky, M.C.S.T. Norovirus: an overview. Rev Assoc Med Bras 57(4):453-458 (2011).
- Preventing Norovirus Outbreaks. http://www.cdc.gov/vitalsigns/norovirus/ (2014)
- Preventing Norovirus Infection. http://www.cdc.gov/norovirus/preventing-infection.html
- MacCannell, T., Umscheid, C.A., Agarwal, R.K., Lee, I., Kuntz, G., Stevenson, K.B. and the Healthcare Infection Control Practices Advisory Committee (HICPAC). Guideline for the Prevention and Control of Norovirus Gastroenteritis Outbreaks in Healthcare Settings. https://www.cdc.gov/hicpac/pdf/norovirus/Norovirus-Guideline-2011.pdf